Strange bedfellows no more: it’s time for research and policy to work together
June 5, 2018
By Dr. Allen Nissenson, KCP Chair
Someone once said, “When you love what you do, you never ‘work’ a day in your life.” But sometimes, it’s a love affair that can drive you mad.
As a physician and researcher for most of my adult life, I’ve spent hundreds upon hundreds of hours chasing objective data, analyzing its importance, and reaching conclusions that – I hope – become helpful and relevant for patients, providers and other researchers. For me, producing good research that fuels innovation and evidence-based practice is incredibly satisfying and – dare I admit it – exciting!
But I also love public policy, particularly healthcare policy. I’ve been fortunate that my career has allowed me the opportunity to be involved in crafting responsible legislation that helps a population of Americans with complex needs. A population with multiple health issues that cry out for smart, outcomes-based, fiscally wise solutions. A population that now represents a true public health crisis driven to a great extent by the growing epidemic of diabetes, obesity, and high blood pressure, among other factors.
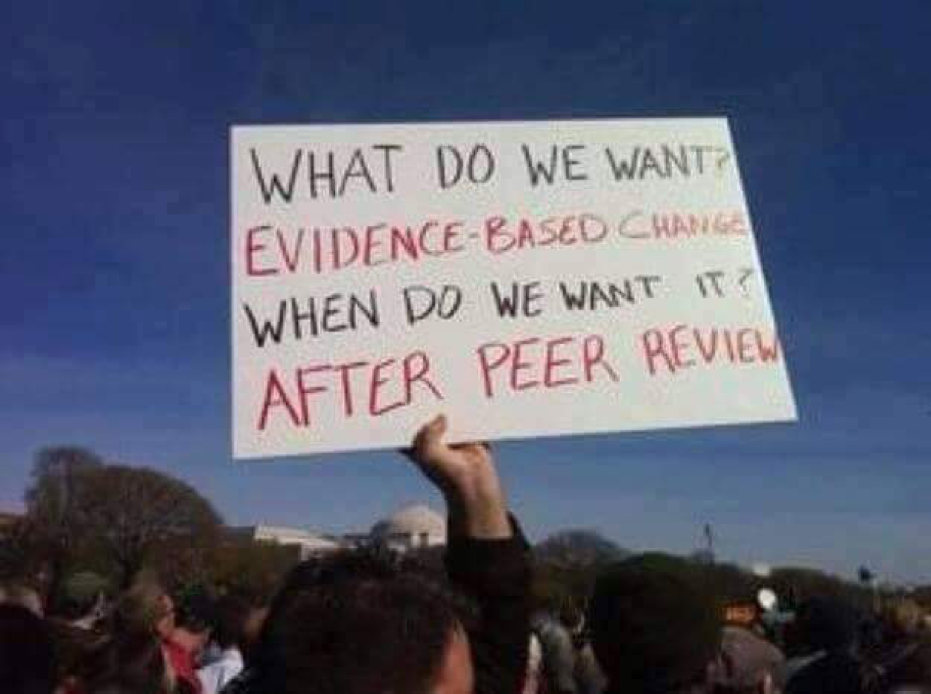
So when I see such a huge chasm between these two things I love – research and policy – it frustrates and saddens me. But it also lights a fire, because I know we can do more!
Research published recently in the Journal of the American Medical Association underscores my frustration.
JAMA’s “Global Burden of Disease Study” evaluated the state of U.S. health between 1990 and 2016 and made frighteningly clear that Chronic Kidney Disease (CKD) is exacting a greater and increasing toll on American lives. CKD ranks 7th as a risk factor for death and ‘disability adjusted life years.’ And since 1990, CKD due to diabetes has climbed from 35th to now the 16th leading cause of death and ‘years of life lost due to premature mortality.’
But even with the explosion of the kidney disease epidemic, our national response has been sadly unremarkable. Research and innovations have lagged due to lack of incentives and coordination commonplace for other disease states with priority focus and coordination among government resources. Policies simply have not kept pace to the extent needed to make real progress. The response is not proportional to the problem – not even close. Especially looking at other conditions such as heart disease, cancer and AIDs, for example, that glean far more attention. Kidney disease has largely been ignored and left in the wake of other diseases, most of which lag the population impact of kidney disease.
Consider the fact that Medicare spends billions of dollars each year caring for kidney disease patient populations, but less than 2 percent of the National Institutes of Health (NIH) budget is spent on kidney disease research. And despite the fact that more than 30 million Americans have CKD today, NIH invests only $13.94 per patient for CKD research, compared to $2,500 per patient for HIV/AIDS research, and approximately $400 per patient for cancer studies.
Now, don’t get me wrong, there is certainly measurable progress being made and the kidney care community—including patients, providers, physicians, device and pharmaceutical manufacturers – deserves its fair share of credit. And this is not just lip service, the United States Renal Data System (USRDS) data clearly show a continued and significant positive trajectory of sustained quality improvements.
For example, the efforts of Kidney Care Partners over the past decade or so working collaboratively with policymakers while also challenging ourselves — has markedly improved quality. The kidney care community has reduced hospitalizations for ESRD patients and saved inpatient Medicare dollars – to the tune of $1.6 billion. We’ve decreased one-year mortality rates by more than 25 percent. We’ve helped improve the adequacy of dialysis, the placement of fistulas, cardiovascular health, and use of patient-empowering modalities such as home dialysis.
It seems like a lot, and it is. But there is so much room to do more. There are so many opportunities to enhance the connections between research and policy, for the benefit of patients and for Medicare.
I was elated earlier this year to learn that exciting, forward-thinking new partnerships might finally close the gap between knowledge and action with CKD and ESRD. The Department of Health and Human Services (HHS) and the American Society of Nephrology recently announced the Kidney Innovation Accelerator (KidneyX) – a program that will seed, incentivize and accelerate breakthroughs in kidney care by providing merit-based, non-dilutive funding to promising innovators through a series of prize competitions. It promises to also establish better coordination among HHS, NIH, the Food and Drug Administration, and the Centers for Medicare & Medicaid Services to break down barriers to innovation.
The potential fruits of KidneyX, paired with hopeful successful passage of the House and Senate versions of the bipartisan The Chronic Kidney Disease Improvement in Research & Treatment Act — could herald a new era for kidney care in this country. The proposals in this legislation would enhance and expand current CKD research efforts and evaluate barriers to care – including initiatives that would involve not only HHS but the National Academy of Sciences and the Government Accountability Office.
All of the research in the world means little, if we can’t transform knowledge into action. As a researcher I’m glad we’re unlocking the unknowns behind CKD and ESRD. And as a lover of policy, I’m excited to see momentum towards using what we know to improve care. The two realms are intrinsically linked, and it’s time we treat them as such.
